Social determinants of health refers to social factors and physical conditions of the environment in which people are born, live, learn, work, and play (e.g., employment, education, social and community context) that affect health and quality-of-life outcomes (1). Social needs, such as transportation, housing, and food security, are encountered at the individual level and reflect how social determinants of health (SDOH) affect individuals’ daily lives. An individual may have a range of social needs that affect their health (2). There is a large body of evidence demonstrating the link between social needs and health, and increasing evidence that addressing individuals’ social needs is associated with improved health outcomes (3, 4). The demonstrated link between social needs and individual health has spurred recent efforts to increase social needs screening and collection of social determinants of health data by providers in inpatient and outpatient settings (5, 6). Hospitals are uniquely suited to help address social needs and assist with transitions of care, particularly those serving high-risk populations. However, it is unclear if these data are collected routinely and whether they are captured in a structured format (i.e., using a screening tool or diagnosis codes) that would facilitate exchange (7). This data brief uses nationally representative survey data from the 2022 American Hospital Association (AHA) Information Technology (IT) supplement to describe the extent to which non-federal acute care hospitals collect and receive data on individual patients’ health-related social needs and how these data are used to promote patient and population health.
HIGHLIGHTS
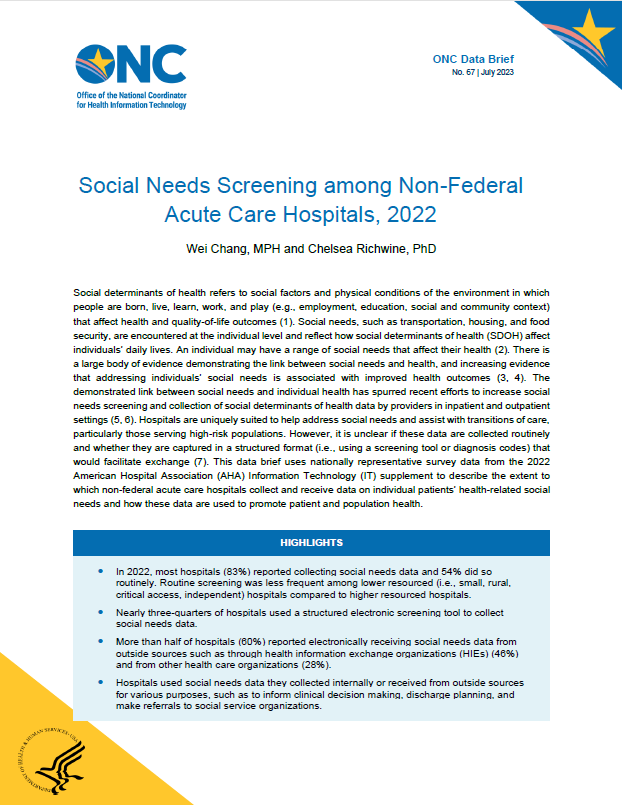
- In 2022, most hospitals (83%) reported collecting social needs data and 54% did so routinely. Routine screening was less frequent among lower resourced (i.e., small, rural, critical access, independent) hospitals compared to higher resourced hospitals.
- Nearly three-quarters of hospitals used a structured electronic screening tool to collect social needs data.
- More than half of hospitals (60%) reported electronically receiving social needs data from outside sources such as through health information exchange organizations (HIEs) (46%) and from other health care organizations (28%).
- Hospitals used social needs data they collected internally or received from outside sources for various purposes, such as to inform clinical decision making, discharge planning, and make referrals to social service organizations.
Most hospitals collected social needs data and more than half electronically received social needs data from outside sources in 2022.
FINDINGS
★ In 2022, 83 percent of hospitals reported collecting data on patients’ health related social needs with 54 percent of hospitals indicating they collect this information routinely.
★ About 60 percent of hospitals reported electronically receiving data on patients’ health related social needs from external sources.
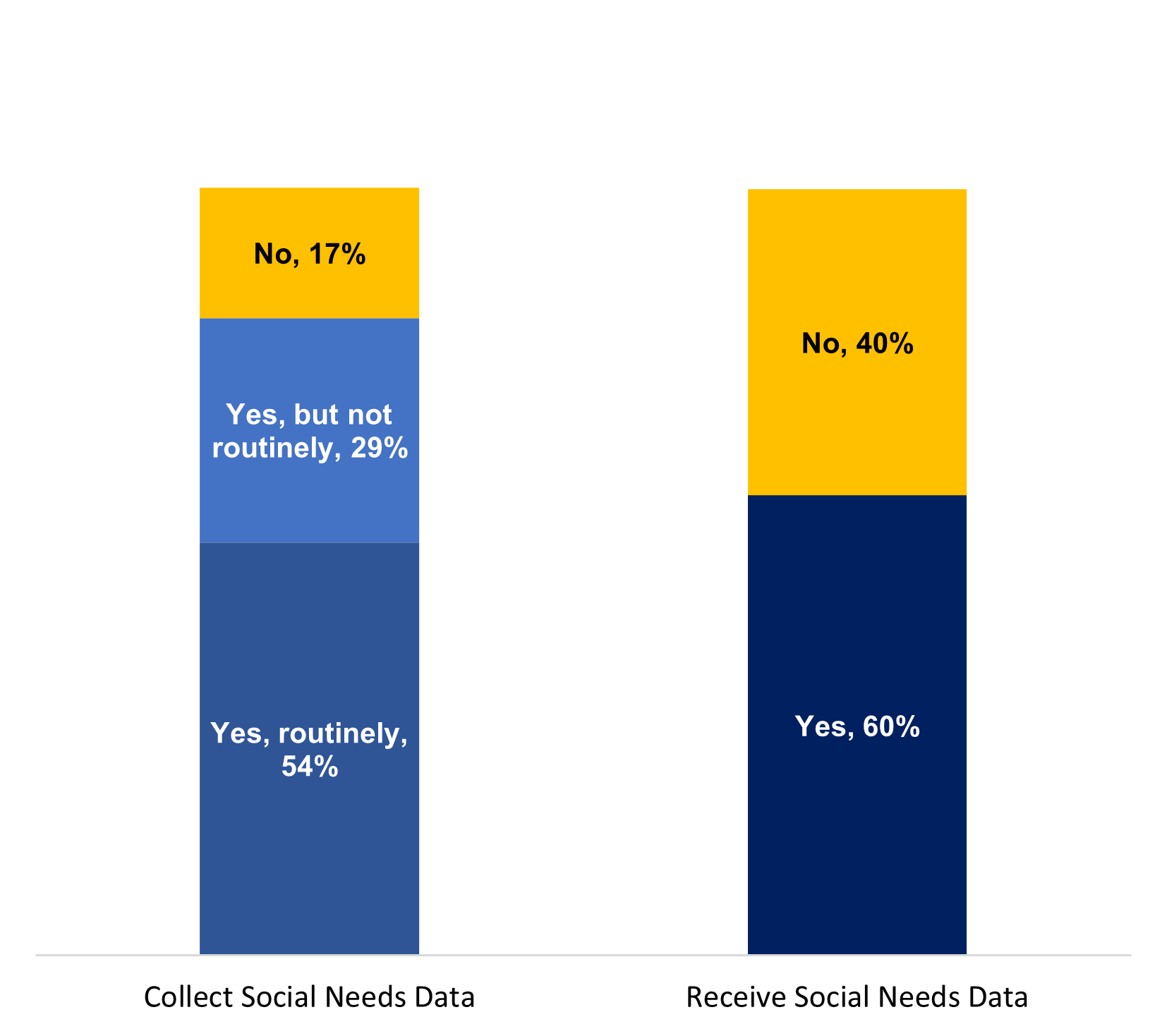
Figure 1: Percent of non-federal acute care hospitals that collected and electronically received data on patients’ health related social needs from external sources, 2022.
Source: 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Notes: These data reflect responses to the survey question “Does your hospital routinely collect data on individual patients' health related social needs (often referred to as social determinants of health) such as transportation, housing, food insecurity or other?” and “From which sources outside your hospital/health system does your hospital electronically receive data on patients’ social needs?” Denominator represents all non-federal acute care hospitals that provide inpatient care. The “No” category includes “don’t know” (N=171 for collect social needs data) and missing responses (N=83 for collect social needs data and N=129 for receive social needs data). See Appendix Table A1 to view survey questions for key measures.
Nearly three-quarters of hospitals used a structured electronic screening tool to collect social needs data.
FINDINGS
★ Among hospitals that reported collecting social needs data, the most common method of data collection was using a structured electronic screening tool (74%), followed by free-text notes(36%), diagnosis codes (29%), and non-electronic methods (20%).
★ Among hospitals that used structured electronic screening tools to collect social needs data, 41percent reported using a combination of customized/home grown tools and externally established tools.
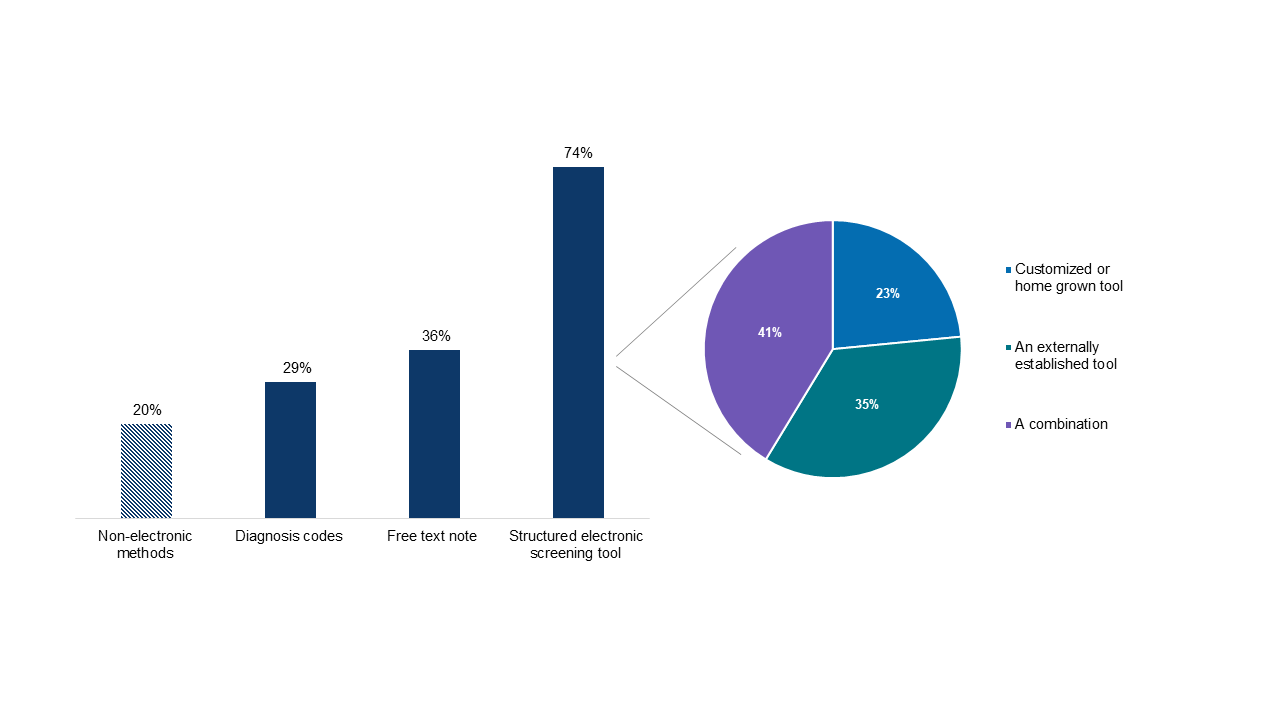
Figure 2: Methods and types of tools used to collect social needs data among hospitals that reported collecting social needs data, 2022.
Source: 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Notes: Data in the bar graph reflect responses to the survey question “How are data on individual patient’s health related social needs recorded at your hospital?” Respondents were instructed to check all that apply and thus responses do not sum to 100 percent. Missing responses were excluded from the denominator (N=18). Data in the pie chart reflect responses to the survey question, “If you use a screening tool, what type of screening tool?” Therefore, the denominator only includes respondents who used a structured electronic screening tool to collect social needs data. Missing and don’t know responses were excluded from the denominator (N=202). See Appendix Table A1 to view survey questions for key measures.
Hospitals’ routine collection of social needs data and collection of data in a structured format varied by hospital characteristics.
FINDINGS
★ About 54 percent of hospitals reported routinely collecting data on patients’ health related social needs and 80 percent of hospitals indicated they collected these data in a structured format (i.e., using a screening tool or diagnosis codes).
★ Lower resourced (i.e., small, critical access, rural, independent hospitals) were significantly less likely to report routinely collecting social needs data compared to their higher resourced counterparts, but collected these data in a structured format at similar rates.
★ While there were few differences in structured screening by hospital characteristics, government and non-profit hospitals were significantly more likely to collect social needs data using a structured screening tool or diagnoses codes compared to for-profit hospitals.
Hospital Characteristics | Collect social needs data routinelya | Use structured screening tool or diagnosis codesb |
|---|---|---|
All hospitals | 54% | 80% |
Small (N = 1,228) | 49%* | 80% |
Medium-Large (N=1,313) | 60% | 80% |
CAH (N=721) | 46%* | 82% |
non-CAH (N=1,820) | 57% | 79% |
Rural (N=648) | 46%* | 82% |
Suburban-Urban (N=1,499) | 61% | 84% |
Independent (N=662) | 44%* | 79% |
System Affiliation (N=1,879) | 59% | 80% |
Minor and Non-teaching Hospitals (N=2,368) | 53%* | 79%* |
Major Teaching Hospital (N=173) | 71% | 96% |
For-profit (N=325)c | 24% | 27% |
Non-profit (N=1,729) | 65%* | 92%* |
Government Owned (N=486) | 41%* | 77%* |
Non-certified EHR (N=119) | 36%* | 77% |
Certified EHR (N=2,422) | 55% | 80% |
Table 1: Routine collection of social needs data and use of structured screening tool or diagnosis codes, by hospital characteristics, 2022.
Source: 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Notes: aDenominator represents all non-federal acute care hospitals that provide inpatient care. bDenominator only includes hospitals that indicated they collect social needs data (N=2,153). cDenotes reference category. *Indicates statistically significant difference from reference group (p<0.05). Please refer to the Definitions section of this data brief for more information on the terminology. See Appendix Table A1 for survey questions for key measures.
Almost half of hospitals reported electronically receiving social needs data through health information exchange organizations (HIEs).
FINDINGS
★ HIEs were the most common method by which hospitals reported electronically receiving social needs data from outside sources.
★ Hospitals also commonly reported receiving social needs data from other health care organizations and through social service or community-based referral platforms.
★ About 40 percent of hospitals reported they did not receive social needs data from any outside sources.
Figure 3: Methods and sources from which hospitals electronically received data on patients’ health-related social needs, 2022.
Source: 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Notes: These data reflect responses to the survey question, “From which sources outside your hospital/health system does your hospital electronically receive data on patients’ social needs?” Denominator represents all non-federal acute care hospitals that provide inpatient care. See Appendix Table A1 to view survey questions for key measures.
Hospitals used social needs data collected internally or received from external sources similarly, with the top 3 uses being to inform clinical decision making, discharge planning, and making referrals.
FINDINGS
★ While the most common uses of social needs data focused on informing clinical decision making and discharge planning for individual patients, social needs data collected internally and received from outside sources were also used for population health analytics (48% and 32%, respectively) and to inform community needs assessments or other equity initiatives (46% and 28%, respectively).
★ Additionaly, 42 percent of hospitals used social needs data collected internally for quality management purposes and a quarter of hospitals reported using social needs data received from outside sources for screening purposes at their hospital.
Purpose | Collect social needs data | Receive social needs data |
|---|---|---|
To inform discharge planning | 72% | 39% |
To inform clinical decision making | 67% | 43% |
For referrals to social service organizations | 65% | 40% |
For population health analytics | 48% | 32% |
To inform community needs assessment or other equity initiatives | 46% | 28% |
For quality management | 42% | — |
For screening at our hospital | — | 25% |
Other | 2% | 1% |
Data not collected or received | 17%a | 40%b |
Table 2: Uses of social needs data collected internally or received from outside sources, 2022.
Source: 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Notes: These data reflect responses to the survey questions: “How does your hospital use data on patients' health related social needs documented at your hospital?” and “If you indicated receiving data on patients' health related social needs from external sources, how do you use these data?” These questions were only asked of respondents who indicated they collected or received data, respectively. Denominator represents all non-federal acute care hospitals that provide inpatient care. Responses do not sum to 100 percent as hospitals were instructed to select all responses that apply. Among respondents who reported collecting social needs data (N=2,153), 31 did not indicate a use of data collected at their hospital. Among respondents who reported receiving social needs data (N=1,570), 65 did not indicate a use of data received by their hospital. a388 hospitals were categorized as not collecting social needs data (134 “Do not collect”, 171 “Don’t know”, and 83 provided no response). b971 hospitals were categorized as not receiving social needs data from outside sources (842 “Do not receive from any sources” and 129 provided no response). See Appendix Table A1 to view survey questions for key measures.
SUMMARY
In 2022, most hospitals (83%) collected social needs data, but only about half (54%) did so routinely. Recently, the Centers for Medicare & Medicaid Services (CMS) added two SDOH measures for hospitals reporting to the Inpatient Quality Reporting (IQR) program to help improve the collection and use of standardized SDOH and social needs data. Hospital reporting on the new measures—which aim to capture the total number of patients that have been screened for SDOH and the share who screened positive in each SDOH category—is voluntary in 2023 and will become mandatory in 2024 (8). While the share of hospitals screening for social needs is relatively high, routine screening was less frequent among lower resourced (i.e., small, rural, critical access, independent) hospitals compared to higher resourced hospitals. The addition of the new social drivers of health measures may help increase the frequency of social needs screening among eligible and critical access hospitals participating in the program and ensure that a certain minimum set of data elements are collected. Future measurement efforts may also leverage FHIR and incorporate standardized data elements for SDOH such as those included in the United States Core Data for Interoperability (USCDI) to further enable interoperable exchange.
Most hospitals that collected social needs data did so using a structured format (i.e., using a structured electronic screening tool, diagnoses codes, or both). Hospitals that used screening tools used customized/home grown tools (23%), externally established tools (35%), or a combination (41%). Methods used by hospitals to collect social needs data varied by consistency of data collection (see Appendix Table A2). Structured electronic screening tools were the most common method used by hospitals that collected social needs data routinely (87%), whereas hospitals that collected social needs data (but not routinely) used structured electronic screening tools and free text notes at the same rate (52%), which suggests a relationship between the consistency and methods of collecting social needs data.
In addition to data collected internally, 60 percent of hospitals electronically received social needs data from sources outside their hospital or health system. HIEs, the most common method by which hospitals’ received social needs data from outside sources, can serve as a powerful data exchange method but require sustainable investment and engagement (9). In addition to data aggregation and data quality services, some HIEs offer more robust tools and services that support clinical decision-making, facilitate communication for care management, and help make connections to community resources (10). However, further investigation is needed to better operationalize the integration of social needs data into health information exchange (11).
In 2022, hospitals used data collected internally and from outside sources similarly, with the top three purposes being to inform clinical decision making, make referrals to social service organizations, and help inform discharge planning. Ongoing measurement will be important to assess whether efforts to improve social needs data collection continues to increase hospitals’ access to information on patients’ health related social needs and expands the use of these data for various purposes, such as improved care coordination and delivery of patient-centered treatment (8, 11).
Our findings suggest that hospitals’ collection of social needs data is widespread, but receipt and usage of data varies. To aid stakeholders interested in improving their collection and use of SDOH data, the Office of the National Coordinator for Health IT (ONC) released a Social Determinants of Health (SDOH) Information Exchange Toolkit that highlights promising approaches for implementing IT infrastructure for SDOH data exchange including the adoption of standards such as Health Level Seven® (HL7) Fast Healthcare Interoperability Resources® (FHIR). The toolkit provides an extensive list of resources and initiatives led or supported by ONC to promote the standardization and exchange of SDOH data, including work done by the HL7 Gravity Project to develop standards for SDOH data and the addition of SDOH data elements to USCDI v2 (12). While our findings suggest social needs data are largely collected in a structured format, future work should assess the extent to which data elements in structured screening tools are mapped to existing standards (e.g., LOINC, ICD-10-CM) as this would enable exchange and use of these data. Continuous measurement of providers’ use of screening instruments will be critical to identifying opportunities to increase the usage of validated and standardized screening tools that align with CMS guidance (13).
DEFINITIONS
Critical access hospital: Hospitals with less than 25 beds and at least 35 miles away from another general or critical access hospital.
Health information exchange (HIE): State, regional, or local health information network. This does not include local proprietary or enterprise networks.
Large hospital: Non-federal acute care hospitals of bed sizes of 400 or more.
Medium hospital: Non-federal acute care hospitals of bed sizes of 100-399.
Non-federal acute care hospital: Hospitals that meet the following criteria: acute care general medical and surgical, children’s general, and cancer hospitals owned by private/not-for-profit, investor-owned/for-profit, or state/local government and located within the 50 states and District of Columbia.
Rural hospital: Hospitals located in a non-metropolitan statistical area.
Small hospital: Non-federal acute care hospitals of bed sizes of 100 or less.
Social determinants of health (SDOH): refers to social factors and physical conditions of the environment in which people are born, live, learn, work, and play (e.g., employment, education, social and community context) that affect health and quality-of-life outcomes (1). At the neighborhood or environmental level, social determinants of health hinder or enhance health through systematic conditions such as the availability of grocery stores and affordable housing (2).
Social needs: Social needs, such as transportation, housing, and food security, are encountered at the individual level. An individual may have a range of social needs that affects their health.(2)
System affiliated hospital: A system is defined as either a multi-hospital or a diversified single hospital system. A multi-hospital system is two or more hospitals owned, leased, sponsored, or contract managed by a central organization. Single, freestanding hospitals may be categorized as a system by bringing into membership three or more, and at least 25 percent, of their owned or leased non-hospital pre-acute or post-acute health care organizations.
DATA SOURCES AND METHODS
Data are from the 2022 American Hospital Association (AHA) Information Technology Supplement to the AHA Annual Survey. Since 2008, ONC has partnered with the AHA to measure adoption and use of health IT in U.S. hospitals. ONC funded the 2022 AHA IT Supplement to track hospital reported adoption and use of EHRs and the exchange of clinical data.
The chief executive officer of each U.S. hospital was invited to participate in the survey regardless of AHA membership status. The person most knowledgeable about the hospital’s health IT (typically the chief information officer) was requested to provide the information via a mail survey or secure online site. Non-respondents received follow-up mailings and phone calls to encourage response.
This brief reports results from the 2022 AHA IT Supplement, which was fielded from July to December 2022. The response rate for non-federal acute care hospitals (N = 2,541) was 58 percent. A logistic regression model was used to predict the propensity of survey response as a function of hospital characteristics, including size, critical access hospital status, location, system affiliation, teaching status, ownership, and EHR certification status. Hospital-level weights were derived by the inverse of the predicted propensity.
REFERENCES
- Office of Disease Prevention and Health Promotion. Social Determinants of Health: U.S. Department of Health and Human Services; [Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health.
- Hacker K, Houry D. Social Needs and Social Determinants: The Role of the Centers for Disease Control and Prevention and Public Health. Public Health Rep. 2022;137(6):1049-52.
- Castrucci BC, Auerbach J. Health Affairs Blog. Available from: https://www.healthaffairs.org/do/10.1377/forefront.20190115.234942/.
- van Beek E, Eckel D, Taylor A. Investing in social services as a core strategy for healthcare organizations: Developing the business case. 2018.
- Richwine C, Charles D, Patel V. Electronic Public Health Reporting & Recording of Social & Behavioral Determinants of Health Among Office-Based Physicians, 2019. 2022.
- Gottlieb LM, DeSilvey SC, Fichtenberg C, Bernheim S, Peltz A. Developing National Social Care Standards. Health Affairs Forefront. February 22, 2023.
- Senathirajah M, Dankwa-Mullan I, Pickens G, Benevent R, Spurlock B. A Hospital Social Needs Index Would Help Hospitals Collaborate To Address Social Needs And Health Equity. Health Affairs Forefront. 2022 AUGUST 2, 2022.
- Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long- Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2023 Rates; Quality Programs and Medicare Promoting Interoperability Program Requirements for Eligible Hospitals and Critical Access Hospitals; Costs Incurred for Qualified and Non-Qualified Deferred Compensation Plans; and Changes to Hospital and Critical Access Hospital Conditions of Participation, (2022).
- How a Michigan HIE is Working Towards SDOH Interoperability: EHR Intelligence [updated September 29, 2022. Available from: https://ehrintelligence.com/features/how-a-michigan-hie-is-working-towards-sdoh-interoperability.
- Social Determinants of Health (SDoH) Data: CRISP; [Available from: https://www.crisphealth.org/learning-system/sdoh-data/.
- S. Allen K, Gilliam NJ, Kharrazi H, McPheeters M, Dixon BE. Chapter 19 - Health information exchange: incorporating social and environmental determinants of health into health information exchange. In: Dixon BE, editor. Health Information Exchange (Second Edition): Academic Press; 2023. p. 423-33.
- Knee M, Gebresellassie M. Office of the National Coordinator for Health Information Technology. [cited 2023]. Available from: https://www.healthit.gov/buzz-blog/public-health/new-releases-sdoh-toolkit-and-learning-forum-sessions-for-the-health-it-community.
- Centers for Medicare & Medicaid Services. List of Screening Instruments for Housing Stability, Food Security, and Transportation Questions on Health Risk Assessments. 2023.
ACKNOWLEDGEMENTS
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology. The data brief was drafted under the direction of Mera Choi, Director of the Technical Strategy and Analysis Division, Vaishali Patel, Deputy Director of the Technical Strategy and Analysis Division, and Wesley Barker, Chief of the Data Analysis Branch with subject matter expertise from Samantha Meklir and JaWanna Henry.
SUGGESTED CITATION
Chang, W., Richwine, C. (July 2023). Social Needs Screening among Non-Federal Acute Care Hospitals, 2022. ONC Data Brief, no.67. Office of the National Coordinator for Health Information Technology: Washington DC.
APPENDIX
Appendix Table A1: Social determinants of health survey questions in the 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Question Text | Response Options |
|---|---|
3. Does your hospital routinely collect data on individual patients' health related social needs (often referred to as social determinants of health) such as transportation, housing, food insecurity or other? |
|
4a. How are data on individual patient’s health related social needs recorded at your hospital? Check all that apply |
|
4b. If you use a screening tool, what type of screening tool? |
|
5. How does your hospital use data on patients' health related social needs documented at your hospital? Check all that apply |
|
6. From which sources outside your hospital/health system does your hospital electronically receive data on patients’ social needs? Check all that apply |
|
7. If you indicated receiving data on patients' health related social needs from external sources, how do you use these data? Check all that apply |
|
Source: 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Appendix Table A2: Methods used to collect social needs data by whether hospitals collect data routinely or not routinely, 2022.
Collect social needs data routinely | Collect social needs data, but not routinely | |
|---|---|---|
Structured electronic screening tool | 87% | 52% |
Free text note | 27% | 52% |
Diagnosis codes | 34% | 20% |
Non-electronic methods | 15% | 29% |
Source: 2022 American Hospital Association (AHA) Information Technology Supplement Survey.
Notes: These data reflect responses to the survey question “How are data on individual patient’s health related social needs recorded at your hospital?” Denominators for “Collect social needs data routinely” and “Collect social needs data, but not routinely) include non-federal acute care hospitals who responded, “Yes, routinely” or “Yes, but not routinely”, respectively, to the survey question, “Does your hospital routinely collect data on individual patients' health related social needs (often referred to as social determinants of health) such as transportation, housing, food insecurity or other?” Missing responses (N=13 for hospitals collecting social needs data routinely and N=5 for hospitals collecting social needs data, but not routinely) were excluded. See Appendix Table A1 to view survey questions for key measures.