In the last decade, the use of artificial intelligence (AI) in health care delivery has grown significantly. Predictive AI, which has been used in health care for decades, leverages machine learning to predict future outcomes for applications such…
Improving seamless, secure public health data exchange between health care and public health remains a key goal of data modernization efforts aimed at ensuring public health agencies (PHAs) have access to timely, accurate data needed to inform…
Family medicine physicians can play an important role in addressing social factors that impact health and health equity (1). Family physicians often provide care for individuals in medically underserved communities (2) and are well-positioned to…
Health information technology standards are used in the health care industry to facilitate the capture and exchange of information.1 Health information exchange organizations (HIOs) are state and regional networks that enable electronic exchange of…
Interoperable laboratory data are critical to ensure the timely and accurate delivery of laboratory test results for clinical decision-making and public health surveillance and monitoring. Interoperable exchange of data has also been shown to reduce…
Seamless interoperable health information exchange between disparate organizations across the health care continuum is crucial to ensure clinicians have access to the most timely and relevent patient health information when making healthcare…
State immunization information systems (IIS), also known as immunization registries, are population-based databases that record vaccinations administered by participating health care providers in a given state (1). Most states require providers to…
The 2020 ONC Cures Act Final Rule implements provisions of the 21st Century Cures Act to require secure access to patient health information through application programming interfaces (APIs), with the goal that more patients would be able to access…
As of January 2022, eligible hospitals and critical access hospitals (CAHs) that participate in the Centers for Medicare & Medicaid Services’ (CMS) Medicare Promoting Interoperability (PI) Program are required to electronically submit data to…
Hospitals play an important role in support of public health functions by contributing timely and accurate data to state and local public health agencies (PHAs). However, the COVID-19 pandemic revealed substantive gaps in our public health…
Amidst a global pandemic, the need for efficient exchange of electronic health information between
hospitals and public health agencies has never been more critical. To ensure public health agencies have
timely and complete data…
Over the past decade, a number of federal health IT policies (1) have sought to advance the interoperable exchange of
electronic health information (EHI) between health care providers. In response to these federal initiatives, health care…
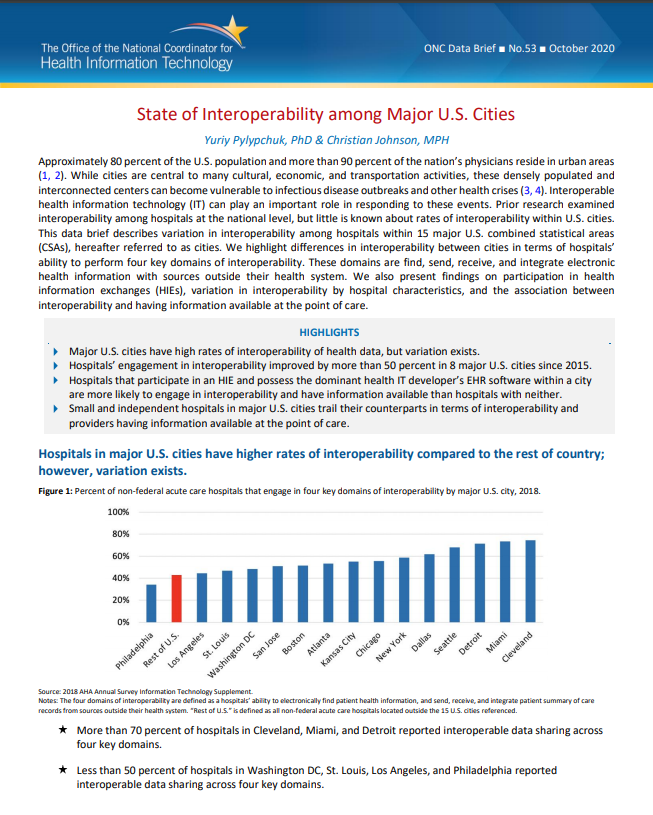
Approximately 80 percent of the U.S. population and more than 90 percent of the nation’s physicians reside in urban areas (1, 2). While cities are central to many cultural, economic, and transportation activities, these densely populated and…
![Variation in Methods for Health Information Management among U.S. Substance Abuse Treatment Centers, 2017 [pdf]](/sites/default/files/2021-07/substance-abuse-treatment-center-health-information-management-2017.png)
More than 20 million Americans suffer from a substance use disorder (SUD) each year. For these individuals, treatment is designed to help stop or reduce harmful substance misuse, improve health and social function, and manage risk for relapse.…
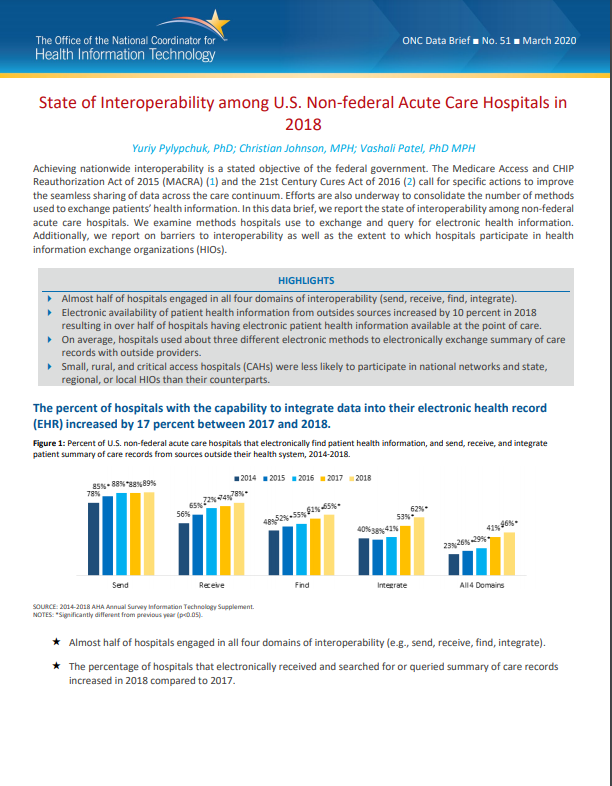
Achieving nationwide interoperability is a stated objective of the federal government. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) ( 1) and the 21st Century Cures Act of 2016 (2) call for specific actions to improve the…
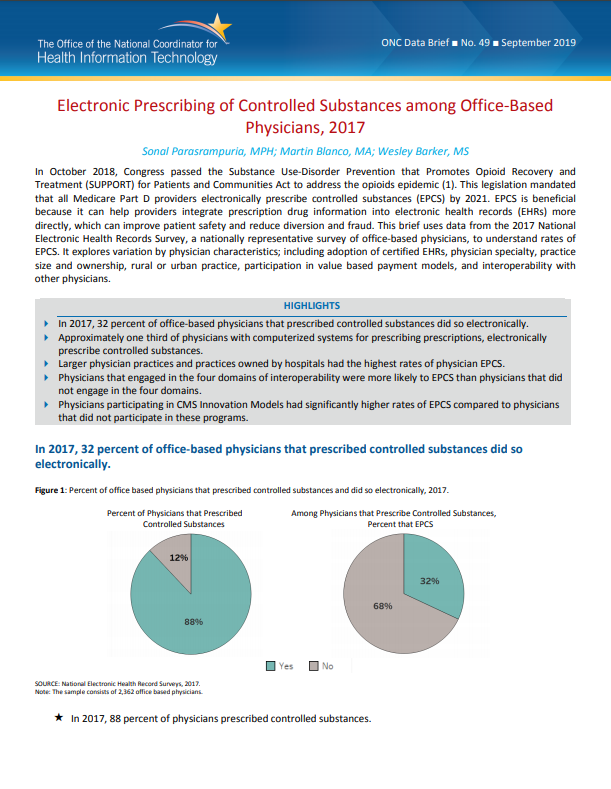
EPCS is beneficial because it can help providers integrate prescription drug information into electronic health records (EHRs) more directly, which can improve patient safety and reduce diversion and fraud. This brief uses data from the 2017…
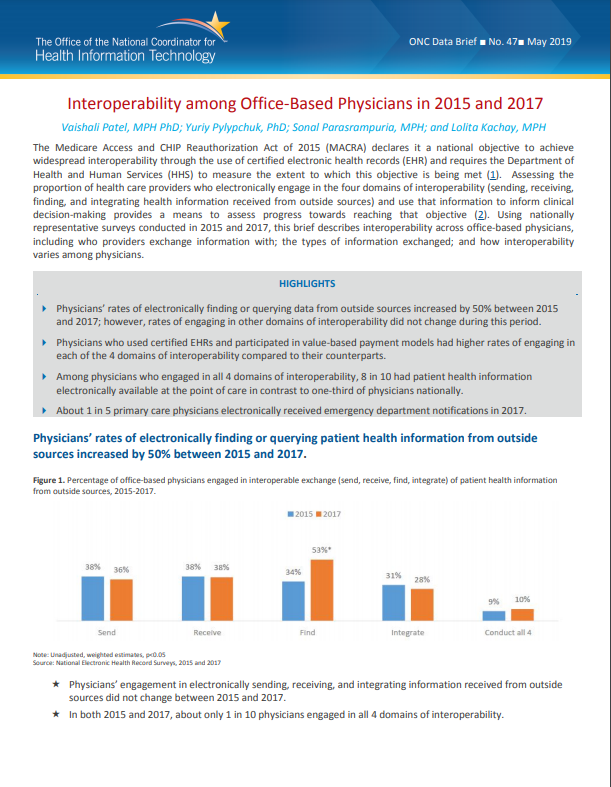
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) declares it a national objective to achieve widespread interoperability through the use of certified electronic health records (EHR) and requires the Department of Health and Human…
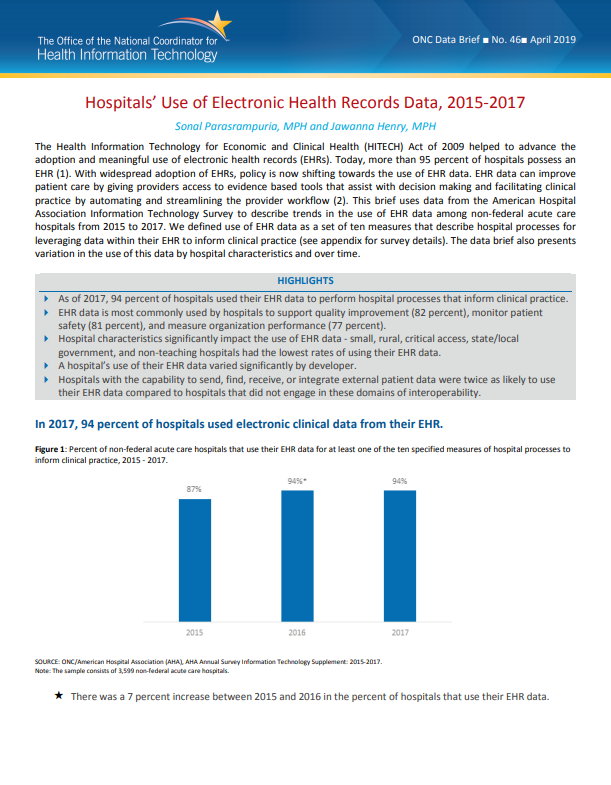
With widespread adoption of EHRs, policy is now shifting towards the use of EHR data. EHR data can improve patient care by giving providers access to evidence based tools that assist with decision making and facilitating clinical practice by…

